Research
Atherosclerosis is the number one cause of death in the United States
Cardiovascular disease (CVD) risk is greatly increased by metabolic diseases such as dyslipidemias and type II diabetes, which continue to increase at an alarming rate world-wide. Since the introduction of the statin class of LDL-lowering drugs over 20 years ago, there have been few significant breakthroughs in the treatment of atherosclerosis. Therefore, there is an unremitting need to better understand the pathogenesis of atherosclerosis and to identify new therapeutic targets for its treatment.
Two approaches are thought to hold particular promise:
Reducing the chronic inflammation that contributes to the progression of plaques and their vulnerability to rupture
Promoting cholesterol efflux from lipid-laden macrophages in plaques and increasing reverse cholesterol transport to promote cholesterol removal from the body.
Our laboratory uses both hypothesis-driven and unbiased approaches to address two outstanding questions:
What underlies the chronic activation of the innate immune system in atherosclerosis and why does resolution of inflammation fail to occur?
How do non-coding RNAs (microRNAs, lncRNAs) regulate lipoprotein metabolism and inflammation, and can these RNAs be manipulated for therapeutic benefit?
By investigating conventional, as well as novel, pathways in innate immunity and lipoprotein metabolism, my research has significantly advanced our knowledge in both of these areas.
First
We discovered new pathways that mediate the innate immune response to altered-self ligands that accumulate in atherosclerosis and Alzheimer’s disease: a new TLR heterodimer (TLR4/TLR6) that mediates the inflammatory response to oxidized-LDL and b-amyloid (Stewart et al. 2010. Nature Immunology), and a CD36-mediated pathway that mediates the intracellular conversion of these soluble ligands into crystals or fibrils that activate the NLRP3-inflammasome and secretion of interleukin-1b (Sheedy et al. 2013. Nature Immunology).
These studies identified long-sought mechanisms for how endogenous ligands that accumulate in atherosclerosis and Alzheimer’s disease trigger chronic innate immune activation.
Second
In the quest to understand why macrophages persist in tissues in atherosclerosis and obesity-induced insulin resistance, we uncovered new roles for neuronal guidance molecule in the pathophysiology of chronic inflammation. We found that netrin-1, originally described as a neuronal guidance cue, acts as a negative regulator of leukocyte migration via its receptor Unc5b (Ly et al. PNAS. 2005).
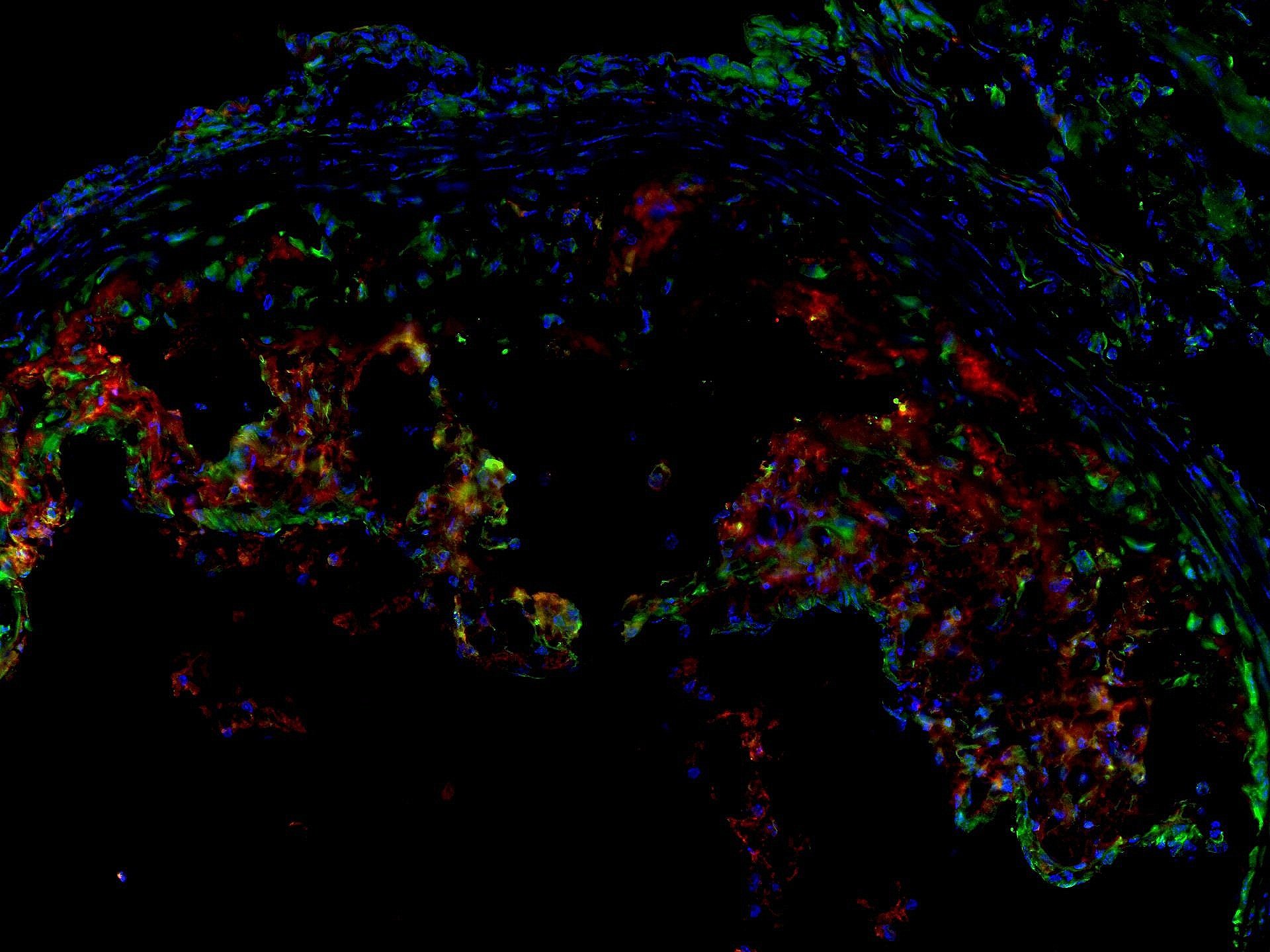
We showed that netrin-1 is highly induced in human and mouse plaque macrophages, which blocks their migration to chemokines directing macrophage exit from plaques (van Gils et al. Nature Immunology, 2012).
Furthermore, we showed that netrin-1 is also induced in the setting of diet-induced obesity and acts to promote macrophage retention in adipose tissue leading to insulin resistance (Ramkhelawon et al. Nature Medicine, 2014).
Furthermore, we showed that netrin-1 is also induced in the setting of diet-induced obesity and acts to promote macrophage retention in adipose tissue leading to insulin resistance (Ramkhelawon et al. Nature Medicine, 2014). Targeting netrin-1 in the plaque can reduce atherosclerotic inflammation and reduce plaque (Schlegel et al. Circulation Research, 2021).
Third
We identified miR-33a and miR-33b as intronic miRNAs of the SREBF2 and SREBF1 genes, and showed that they cooperate with their host gene products to balance cellular lipid levels. We showed that miR-33 represses cholesterol efflux, HDL biogenesis and fatty acid oxidation, and that targeting of miR-33 in mice and non-human primates raised plasma HDL, lowered triglycerides, and regressed atherosclerosis (Rayner et al. 2010. Science; Rayner et al. 2011. J. Clin. Invest; Rayner et al. 2011. Nature).
These findings broke open the field of miRNA regulation of lipoprotein metabolism, and showed the potential of miRNAs as therapeutic targets in atherosclerosis. Since those initial discoveries, we have also shown that miR-33 regulates macrophage inflammatory polarization by altering cellular immumetabolism (Ouimet et al. J. Clin. Invest, 2015); and that Mycobacterium tuberculosis induces the miR-33 locus to repress macrophage autophagy and fatty acid metabolism to promote intracellular bacterial survival (Ouimet et al. Nature Immunology, 2016).
Fourth
We established that myocardial infarction can induce systemic alterations that imprint innate immune memory, altering subsequent immune responses to drive cross-disease communication in CVD and cancer. With the growing recognition that breast cancer survivors have increased CVD risk, we investigated whether incident CV events could alter cancer pathogenesis. We found that breast cancer survivors who experienced CV events had a 60% increased risk of cancer recurrence and cancer-specific mortality (Koelwyn et al. 2020. Nat Med). Using mouse models of breast cancer, we found that myocardial infarction accelerates breast cancer outgrowth by epigenetically reprogramming monocytes in the bone marrow reservoir to an immuno-suppressive phenotype that is maintained upon recruitment to tumors, where these cells established a pro-tumorigenic immune environment. These findings highlight the complex bi-directional relationship between cancer and CVD, and the need to implement strategies to mitigate CVD risk in patients with breast, and potentially other forms of, cancer.
Taken Together
These innovative studies have had important impacts, ranging from new insights into innate immunity and lipid metabolism to the identification of novel therapeutic targets for CVD. Each of these seminal discoveries has opened up new avenues for exploration of atherosclerosis and other inflammatory diseases, and they form the basis for our continuing research efforts.
